Why covid-19 might finally usher in the era of health care based on a patient’s data
Back in the 1990s, Lee Hood, a technologist and immunologist famous for co-inventing the automated DNA sequencer, made a bold prediction. By 2016, he suggested, all Americans would carry a data card recording their personal genomes and medical histories in vast detail. Upon arriving at a hospital or doctor’s office, they would present it to a clinician, who could simply insert the card into a computer and “instantly know what he’s dealing with.”
Twenty-five years later, Hood’s vision of precision health care based on personalized data still seems a long way off. Too bad, because we could really have used it in the covid-19 pandemic.
Infectious diseases don’t get much more personalized than covid-19. No one can explain with any certainty why seemingly similar individuals respond so differently to exactly the same pathogen. Why do some of us get a case of the sniffles, and others end up on a ventilator? How can the virus attack the lungs of one patient, the heart of another, and the nervous system of a third? Why are so-called long-haulers left with lingering problems, yet other people recover fully? Why do some never show symptoms at all?
It’s hard not to wonder whether we’d already have solved these mysteries if the first covid patients had arrived at the hospital with Hood’s medical cards full of health data. “I think we’d be much further along than where we are right now,” he says.
The dream of true precision medicine has been mired in the sluggish and recalcitrant health-care system, where patient data is often seen as more of a nuisance than a benefit.
But Hood, who is 83, has never been one to dwell on what could have been. Known for his scientific ambition and impatience—he left a safe, tenured university job at 61 to cofound the Institute for Systems Biology (ISB), a nonprofit biomedical research center in Seattle—he sees the pandemic as a once-in-a-lifetime opportunity to show the power of data to help us understand disease. He hopes it will reinvigorate his three-decade-long campaign for a transformation of health care.
Hood, like the many other researchers who have long advocated for such a shift, argues that our approach to medicine is too cookie-cutter. By and large, people with the same illness get the same treatment. This fails to account for big differences between different people’s genomes and immune systems. But the dream of true precision medicine has been mired in the sluggish and recalcitrant health-care system, where patient data is often seen as more of a nuisance than a benefit.
Could the covid crisis finally shake things loose?
The covid data deluge
Last March, Hood and ISB’s president, Jim Heath, launched an ambitious effort to answer the question of why people respond so differently to covid-19. Their study is shaping up to be one of the world’s most comprehensive analyses of the human immune response to the virus.
“This absolutely validates everything I have been arguing for the past 20 years.”
The ISB team collected multiple blood samples from each of several hundred hospitalized covid patients as they progressed through the various stages of the disease. Then the researchers tracked each patient’s immune response down to the molecular level, analyzing a total of 120,000 variables. They looked at different types of immune cells, determined whether the cells were activated, exhausted, or quiescent, and examined the distinct characteristics of the proteins on those cells’ surfaces that allow them to bind to and attack the virus.
The team at ISB also sequenced the patients’ genomes, pulled electronic medical histories, analyzed their complete protein profiles and “metabolomes” (the set of various molecules other than proteins in the samples), and applied the latest pattern-recognition and machine-learning techniques to compare the patients with each other and with healthy people of similar ages.
The first results from this vast effort appeared in the journal Cell last fall, and they contained some surprising insights. Most notable was that as some patients progress from mild to moderate stages of the disease, they undergo a shift: a drop in the availability of key metabolites needed to power an effective immune response. In short, the body seems to just run out of the raw materials needed to fight back. That means something as simple as dietary changes or nutritional supplements might help gird up weak immune systems.
“There’s nothing more personal than your immune system,” says Mark Davis, a Stanford immunologist and a collaborator on the study. Davis notes that our immune system is highly plastic and responsive to past experiences—so much so that 70% of its measurable components differ between identical twins just a couple of years after birth.
Davis believes the key to understanding why covid affects people in such varied ways is to identify the differences between the immune systems of those who successfully fight the disease and those who succumb. Those differences could range from the simple, such as whether someone has been exposed to other coronaviruses in the past, to factors as complex as genetically determined variations in how certain cells display viral protein fragments on their surfaces for inspection by circulating immune cells. These proteins can influence how likely the immune cell is to recognize the presence of a dangerous pathogen, sound the alarm, and mobilize an army of antibodies to go on the attack.
“Now there is a flood of data, and it’s the highest quality that we’ve ever had, and also the most we’ve ever had,” Davis says.
A boon for the science, to be sure. But will the ISB study change how patients are treated and help prepare us for future pandemics? Hood is optimistic. “This absolutely validates everything I have been arguing for the past 20 years,” he says.
The needed tools
Hood made a major contribution to immunology early in his career, after attending medical school and getting his PhD from Caltech. He helped solve the mystery of how the body can produce roughly 10 billion varieties of antibodies, Y-shaped proteins that can bind to the outer surface of a distinctly shaped invading pathogen and destroy it with the specificity of a guided missile.
Despite his early success, Hood recognized from the start that without major advances in technology, he would never answer the most intriguing biological questions that remained about the immune system: those revealing how it coordinates its remarkably complex collection of cell types and proteins. If immunologists were ever to understand how all these parts worked together, Hood realized, they would first need to recognize, characterize, and measure them.
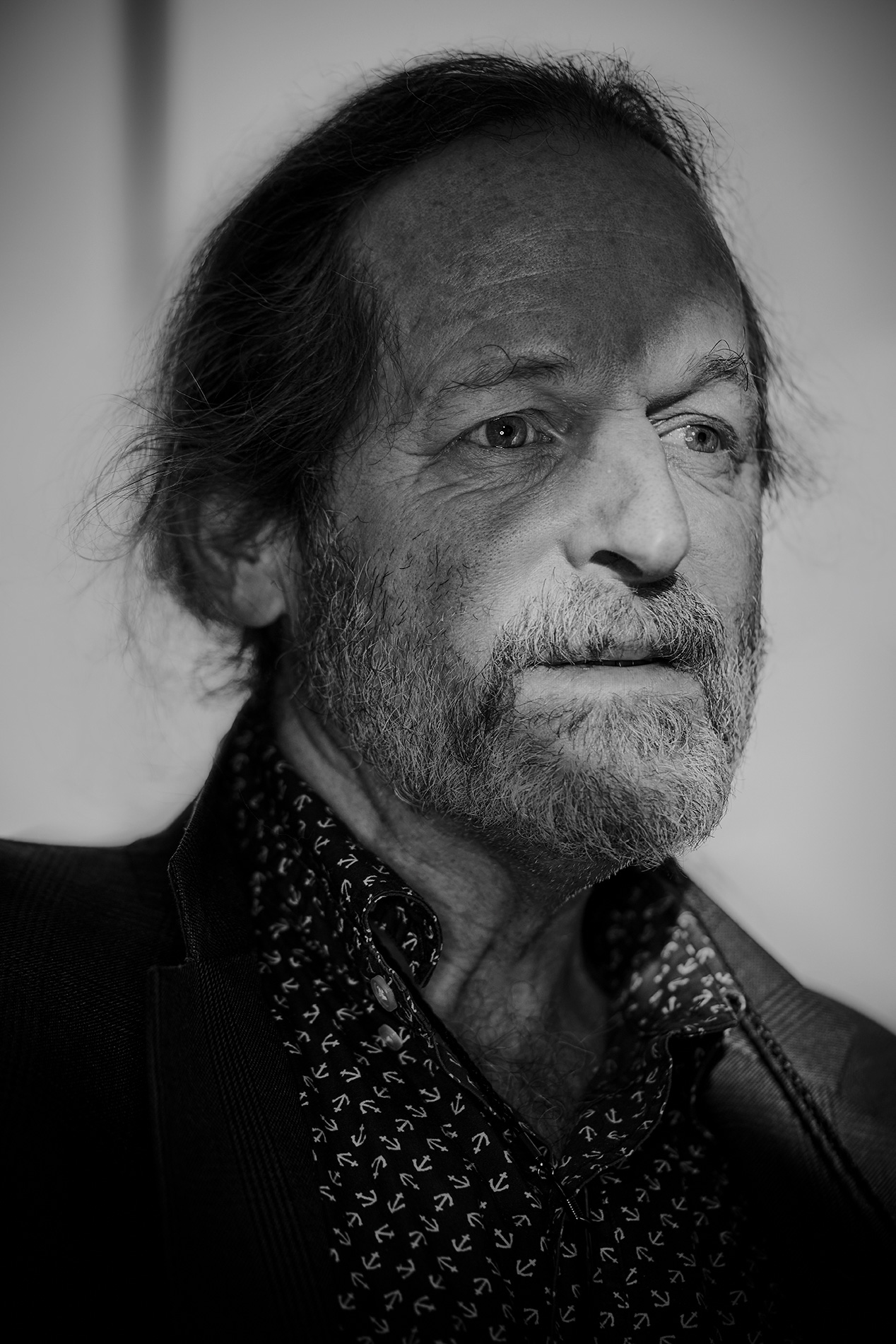
Hood’s Caltech lab played a key role in developing a wide range of tools, including instruments that would enable biologists to read and write sequences of amino acids, and machines that could string together DNA nucleotides (the letters of the genetic code). Perhaps most famously, in 1986 he helped invent the automated DNA sequencer, a machine able to quickly read the nucleotides in the genome and determine their order; it paved the way for the Human Genome Project, the $3 billion, 13-year effort to produce the first draft of a complete human genome.
In the years that followed, Hood advocated for a reinvention of modern health care that relied on the new tools of molecular biology to collect data from individual patients: genome sequences, and complete inventories of proteins circulating in the bloodstream. This data could then be analyzed, using early systems of machine learning and pattern recognition to pull out interesting patterns and correlations. Insights could be harnessed to maximize a person’s health and head off diseases far earlier than previously possible.
It all made perfect scientific sense. But nearly two decades after the Human Genome Project’s completion in 2003, and despite much progress in genomic sciences as well as in data science, Hood’s predicted revolution in health care has still not arrived.
Hood says one reason is that the tools used to be expensive. Now, however, a genome can be sequenced for $300 or less. And, he says, researchers have gained access to computational tools “that can really integrate the data, and turn data into knowledge.”
But the biggest roadblock is that the health-care system is inefficient and resistant to change. There’s a “lack of understanding about how important it is to get diverse types of data and integrate them,” Hood says. “Most physicians went to medical school five or 10 or 20 years ago, and they never learned anything about any of this.”
“Everybody is really busy, and changing takes time, so you have to persuade leadership as well as physicians this is in their interest,” he says. “That all turned out to be far more difficult than I ever thought it would be.”
Pandemic lessons
These days, Hood is still pushing hard, and despite the years of frustration, he is characteristically optimistic. One reason for his renewed hope is that he finally has ready access to patients and the money to begin his next grand experiment.
In 2016, ISB merged with Providence Health & Services in Seattle, a massive network with 51 hospitals, billions of dollars in cash, and a hunger to develop a more robust research program.
Soon after the merger, Hood was talking up an impossibly ambitious-sounding campaign to start what he calls the Million Person Project. It would apply phenotyping and genetic analysis to, yes, a million people. In January 2020, Hood kicked off a pilot project, having recruited 5,000 patients, and began to sequence their genomes.
Then the first covid cases began arriving in the hospital.
Hood and Jim Heath had a video call with Roger Perlmutter, an ISB board member who oversaw the $10 billion research budget of the pharmaceutical behemoth Merck. They discussed what was known about the mysterious new disease—and, more important, what scientific questions most urgently remained to be answered.
It did not take long for the trio of scientists to home in on the challenge.
“The immediate question then—it’s still the question now, frankly—was why is it that there are many people infected, but only a few become very, very ill?” Perlmutter says. “And what is the nature of the transition from … what is often an asymptomatic or mildly symptomatic infection to a catastrophic illness? What does it look like? And how can we understand it from a molecular cell-biology perspective?”
On the call that day, Hood and Heath had a big ask: would Perlmutter finance them to conduct the kind of comprehensive molecular-level analysis that might explain covid’s remarkable variability?
“I don’t ordinarily say, when somebody calls me up, ‘Yeah, sure, I’ve got my checkbook—here we are, let’s do it,’” Perlmutter recalls. “But I said we would be prepared to underwrite it on that call. We needed the data. And I didn’t want to see them struggling to raise money when we needed the data.”
“[Covid] showed, clearly, that you can really get things done at lightning speed if there’s urgency behind them.”
Lee Hood
At Providence, which was filling up with covid patients, the urgency was similarly palpable. The team at ISB began collecting data to characterize the patients’ immune responses with unprecedented specificity. As it happened, Heath and his team already had a powerful array of instruments for the purpose: they were studying ovarian and colorectal cancer patients in danger of recurrence, in hopes of developing better immunotherapies to treat them.
“Ordinarily,” says Hood, “a trial like that would take six months at least to put in place, but in two to three weeks, it was actively ongoing. We were recruiting patients, and drawing the blood, and beginning to test them.”
Though Hood’s Million Person Project was shut down temporarily when covid hit, he has kept his focus on the long game. “What covid has made possible is it’s allowed me to go out and raise really close to $20 million to carry out these studies,” he says. “Part of it was used to build computational platforms and bring in key data scientists. All of these people will be able, once covid’s over, to apply directly to the Million Person Project.” He goes on, “We’ll probably be setting up clinical trials using deep phenotyping for a whole series of diseases in the future.”
Such a prediction is pure Hood, shaped both by his ambition and his endless enthusiasm, even after almost 30 years of advocating for personalized medicine with seemingly little progress.
Even if his grand vision is realized, it will be too late to save us from the worst effects of covid-19. But Hood clearly relishes the opportunity the pandemic has created. “[Covid] showed, clearly, that you can really get things done at lightning speed if there’s urgency behind them,” he says. “Usually it takes forever to get things done. But in a crisis you just push aside all the bureaucracy.”

