The quest to show that biological sex matters in the immune system
Sabra Klein is deeply aware that sex matters. During her PhD research at Johns Hopkins University, Klein learned how sex hormones can influence the brain and behavior. “I naively thought: Everybody knows hormones can affect lots of physiological processes—our metabolism, our heart, our bone density. It must be affecting the immune system,” she says.
But when she graduated in 1998, she struggled to convince others that sex differences in the immune system were a worthy topic for her postdoctoral research. “I wasn’t able to find a microbiologist or an immunologist who was going to let me study sex differences,” she says.
She ultimately found a postdoctoral position in the lab of one of her thesis committee members. And in the years since, as she has established a lab of her own at the university’s Bloomberg School of Public Health, she has painstakingly made the case that sex—defined by biological attributes such as our sex chromosomes, sex hormones, and reproductive tissues—really does influence immune responses.
Through research in animal models and humans, Klein and others have shown how and why male and female immune systems respond differently to the flu virus, HIV, and certain cancer therapies, and why most women receive greater protection from vaccines but are also more likely to get severe asthma and autoimmune disorders (something that had been known but not attributed specifically to immune differences). “Work from her laboratory has been instrumental in advancing our understanding of vaccine responses and immune function on males and females,” says immunologist Dawn Newcomb of the Vanderbilt University Medical Center in Nashville, Tennessee. (When referring to people in this article, “male” is used as a shorthand for people with XY chromosomes, a penis, and testicles, and who go through a testosterone-dominated puberty, and “female” is used as a shorthand for people with XX chromosomes and a vulva, and who go through an estrogen-dominated puberty.)
Through her research, as well as the unglamorous labor of arranging symposia and meetings, Klein has helped spearhead a shift in immunology, a field that long thought sex differences didn’t matter. Historically, most trials enrolled only males, resulting in uncounted—and likely uncountable—consequences for public health and medicine. The practice has, for example, caused women to be denied a potentially lifesaving HIV therapy and left them likely to endure worse side effects from drugs and vaccines when given the same dose as men.
Men and women don’t experience infectious or autoimmune diseases in the same way. Women are nine times more likely to get lupus than men, and they have been hospitalized at higher rates for some flu strains. Meanwhile, men are significantly more likely to get tuberculosis and to die of covid-19 than women.
In the 1990s, scientists often attributed such differences to gender rather than sex—to norms, roles, relationships, behaviors, and other sociocultural factors as opposed to biological differences in the immune system.
For example, even though three times as many women have multiple sclerosis as men, immunologists in the 1990s ignored the idea that this difference could have a biological basis, says Rhonda Voskuhl, a neuroimmunologist at the University of California, Los Angeles. “People would say, ‘Oh, the women just complain more—they’re kind of hysterical,’” Voskuhl says. “You had to convince people that it wasn’t just all subjective or environmental, that it was basic biology. So it was an uphill battle.”
Despite a historical practice of “bikini medicine”—the notion that there are no major differences between the sexes outside the parts that fit under a bikini—we now know that whether you’re looking at your metabolism, heart, or immune system, both biological sex differences and sociocultural gender differences exist. And they both play a role in susceptibility to diseases. For instance, men’s greater propensity to tuberculosis—they are almost twice as likely to get it as women—may be attributed partly to differences in their immune responses and partly to the fact that men are more likely to smoke and to work in mining or construction jobs that expose them to toxic substances, which can impair the lungs’ immune defenses.
How to tease apart the effects of sex and gender? That’s where animal models come in. “Gender is a social construct that we associate with humans, so animals do not have a gender,” says Chyren Hunter, associate director for basic and translational research at the US National Institutes of Health Office of Research on Women’s Health. Seeing the same effect in both animal models and humans is a good starting point for finding out whether an immune response is modulated by sex.
But you can’t find sex differences if you’re only studying one sex. Klein remembers a meeting where a researcher on nematodes, a type of parasitic worm, mentioned that his experiments were done only in male mice, because female mice didn’t get infected. She recalls being flabbergasted that he never thought to study why the nematodes couldn’t infect the females. “Oh my God, you might have a cure for these nematodes that wreak havoc!” she recalls thinking.
In 1992, the US Food and Drug Administration approved a medication called Ambien to help people sleep. It later became clear that the active ingredient in the drug, zol-pidem, could cause some serious complications, including “sleep driving”—like sleepwalking, but potentially far more dangerous. By 2013, laboratory studies and driving simulations had shown that eight hours after taking zolpidem, women were more likely than men to have enough of the drug left in their blood to impair driving and increase their risk of traffic accidents. That year, the FDA set the drug’s dosage for women at half the level for men. Studies in both animals and humans showed that females take longer to metabolize the drug and are more susceptible to its effects.
Ignoring such differences prior to a drug’s approval can increase the risk of harmful, and potentially even life-threatening, effects. That is assuming those differences are studied in the first place; historically, the vast majority of clinical trials enrolled primarily men. Women often bore the worst of the side effects. Between 1997 and 2001, eight out of 10 drugs that the FDA pulled from the market were found after approval to pose greater health risks in women. “The drugs that came on the market were really for men,” says Rosemary Morgan, one of Klein’s colleagues at Hopkins.
Preclinical animal studies, which are often precursors to clinical trials, have a similarly bad track record. As recently as five years ago, more than 75% of rodent drug studies were conducted only on males.
It can take more effort—and money—to study animals of both sexes. Many scientists avoid female animals because they don’t want to account for their reproductive cycles, even though studies have shown that female mice, rats, and hamsters are no more variable—and in some cases are less variable—than their male counterparts in traits ranging from gene expression to hormone levels. Other researchers use only females, because males are more likely to fight when you put them together in a cage. (Klein says researchers can get around this by obtaining male animals before puberty and letting them grow up together for a few weeks.)
“If you’ve got this situation where there’s two groups that have a difference, that’s like a gold mine for discovery.”
In the mid-1990s, Voskuhl made good use of both male and female mice to investigate why females were so much more susceptible to autoimmune diseases such as lupus and multiple sclerosis. There was a well-studied mouse model of multiple sclerosis, but up until that point most researchers had focused on how the disease progressed in female mice, because the males didn’t get as sick. Voskuhl zeroed in on that difference. Among other things, she transferred immune cells from mice of one sex to mice of the other and found that immune cells derived from females were more likely to induce the disease than immune cells from males.
The finding helped make it clear that biological sex also affects susceptibility to multiple sclerosis (other factors, like gender, may also play some role; women are, for example, generally more likely to seek health care). “It showed that there were very basic biological differences,” Voskuhl says. That’s important, because showing that sex is a factor is a necessary precursor to investigating the immune mechanisms at work.
By the mid-1990s, the clinical trial situation was also improving. In 1993, the US Congress passed a law requiring that women be included in all clinical research funded by the NIH. As for animal studies, in 2016 the NIH instituted its “Sex as a Biological Variable” policy, mandating that grant applications consider sex in the design, analysis, and reporting of research in vertebrate animals and humans. Similar policies had already been enacted in Canada and Europe, but the NIH is the world’s largest public funder of biomedical research.
But these changes were just a start—especially in immunology, which in a 2011 review had ranked last out of 10 biological disciplines for reporting the sex of human or animal subjects in published papers.
In 2010, for example, Klein reanalyzed publicly available data on a long-standing, highly effective vaccine for yellow fever. The researchers who generated the data hadn’t analyzed it by sex. When Klein did, she found a previously undetected difference in the immune response to the vaccine, with females experiencing a stronger response and potentially better protection. “That really stands out as a great contribution to the field and really showed the value of analyzing data stratified by sex,” Benn says. “The overall kind of blurry result was actually covering some very significant differences in responses between males and females.”
Around that same time, Klein had set her sights on an enduring mystery—why women tended to have better protection from flu vaccines and more severe responses to the flu. Klein found that female mice infected with flu typically have more inflammation and tissue damage in their lungs than males, and more severe outcomes overall, as a result of their stronger immune response. “Pick an immune response, and our female mice mount significantly higher immune responses than males,” she says.
Klein’s work suggests that these biological sex differences affect how we respond to viruses. Women are known to report more adverse events after vaccines, and this has long been thought to be due to gender rather than sex—for example, maybe men are reluctant to report such events, or women are more likely to report perceptions of pain. But by the late 2000s, Klein and others showed that in addition to any such differences, females need far less vaccine to mount the same antibody response as males.
These findings were “really groundbreaking,” Benn says. “That seems quite clear from the research that Sabra has done, and others, that we need perhaps to have sex-differential vaccination programs.”
Giving women a lower dose of the flu vaccine, which could be equally effective while reducing side effects, could potentially reduce vaccine hesitancy. Klein has advocated for such a policy in numerous lectures, interviews, and scientific articles, as well as in a 2009 New York Times op-ed titled “Do Women Need Such Big Flu Shots?” So far, however, the idea has gained little traction.
Benn suggests multiple reasons why it hasn’t caught on, including the fact that it can seem counterintuitive to treat the sexes differently in order to ensure similar outcomes. “Researchers can come to an agreement about such things long before policymakers start moving there,” she says. “And you can also see that administratively, it might be a bit more complicated.”
The same heightened immune responses that help keep babies alive also increase the risk of autoimmune diseases.
But Klein points out that it wouldn’t be that different from giving people over 65 a higher dose of the flu vaccine than younger adults, something we already do.
Women aren’t the only ones who might benefit from vaccine policies that account for sex differences. Janna Shapiro, who recently completed her PhD with Klein and Morgan, found that older males who received flu or covid vaccines showed a much more drastic decline in vaccine-induced immunity over time than older females. Not only is the third dose of the covid vaccine particularly important for older males, but Shapiro suggests that they might greatly benefit from a midseason flu booster shot, even though there’s currently no such shot available to them.
A stronger female immune response shows up in many different species, from sea urchins and fruit flies to birds and rodents to macaques and humans. “If we were to kind of take a Darwinian perspective, there must be some type of evolutionary reason why these differences have evolved,” Klein says.
One hypothesis suggests that a stronger immune response in female mammals could help transfer more antibodies to their babies in utero and through their milk, thus protecting offspring from infections. The same heightened immune responses that help keep babies alive also increase the risk of autoimmune diseases when females are older, but the trade-off may be worth it from an evolutionary standpoint.
Within our genomes, the sex differences in the immune system often play out on the X chromosome, which hosts a large number of genes involved in immune signaling and response. “Having two Xs really differs in terms of immune issues from an X and a Y,” says Marcia Stefanick, director of the Stanford Women’s Health and Sex Differences in Medicine Center in California. Two X chromosomes can mean twice as many copies of some of these immune genes. In principle, only one copy should be active, but in practice, the result is higher gene expression and a stronger immune response.
The X chromosome gene called TLR7, or toll-like receptor 7, has been implicated in a number of immunological sex differences. TLR7 plays an important role in recognizing pathogens and activating the immune system, and it may contribute to higher female prevalence of autoimmune diseases, particularly lupus. “If we eliminate TLR7, we eliminate that female-biased immunity and protection following vaccination,” says Klein.
TLR7 may also play a role in explaining why women tend to have a stronger immune response to HIV than men. Researchers didn’t know about this immunological sex difference in the 1990s, when decisions on who was eligible for HIV therapy were sometimes based on how much virus you had—your “viral load,” says Scully. But it is the immune response and not the viral load that is the dominant predictor of the progression of HIV to AIDS. That meant many women who should have received treatment did not.
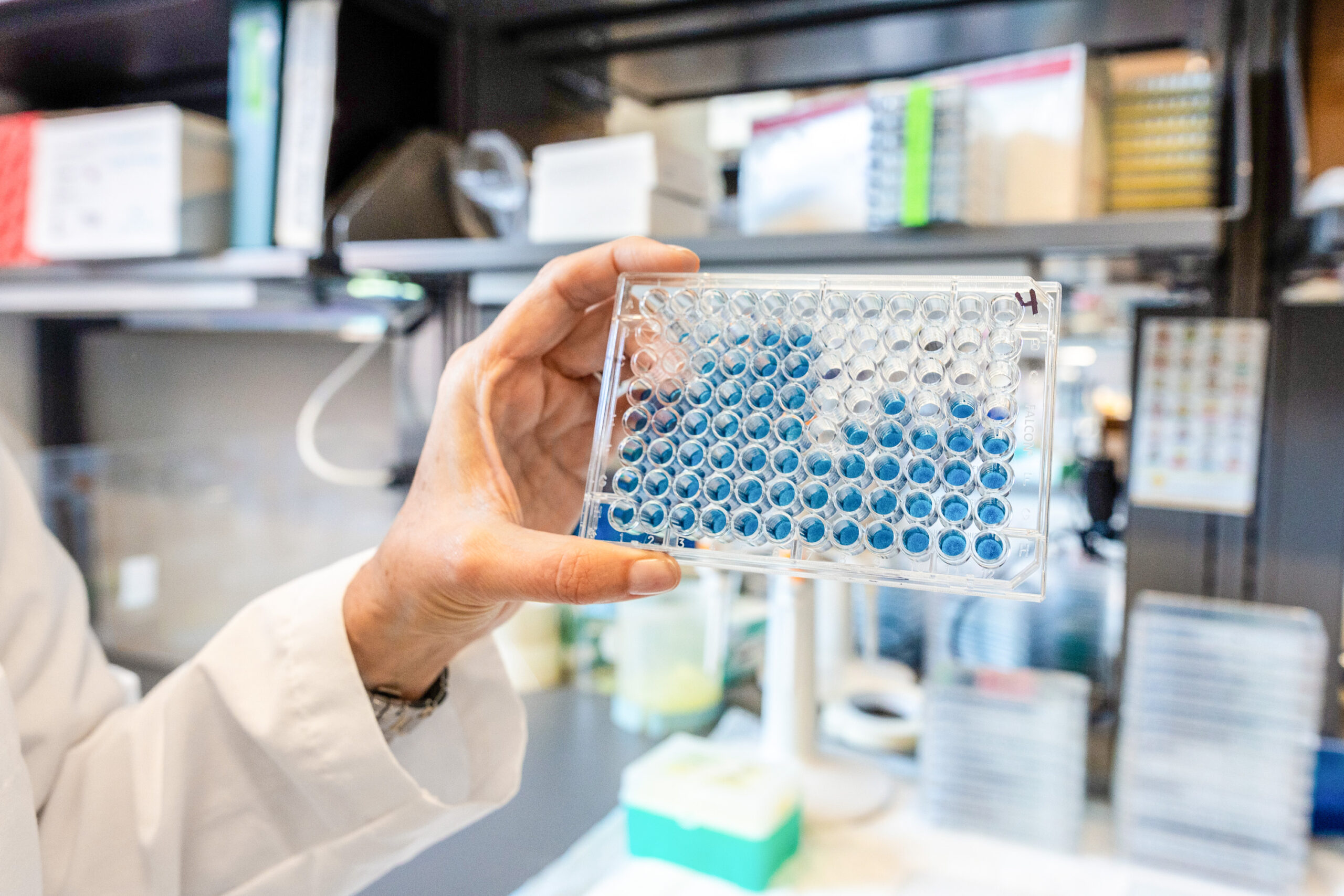
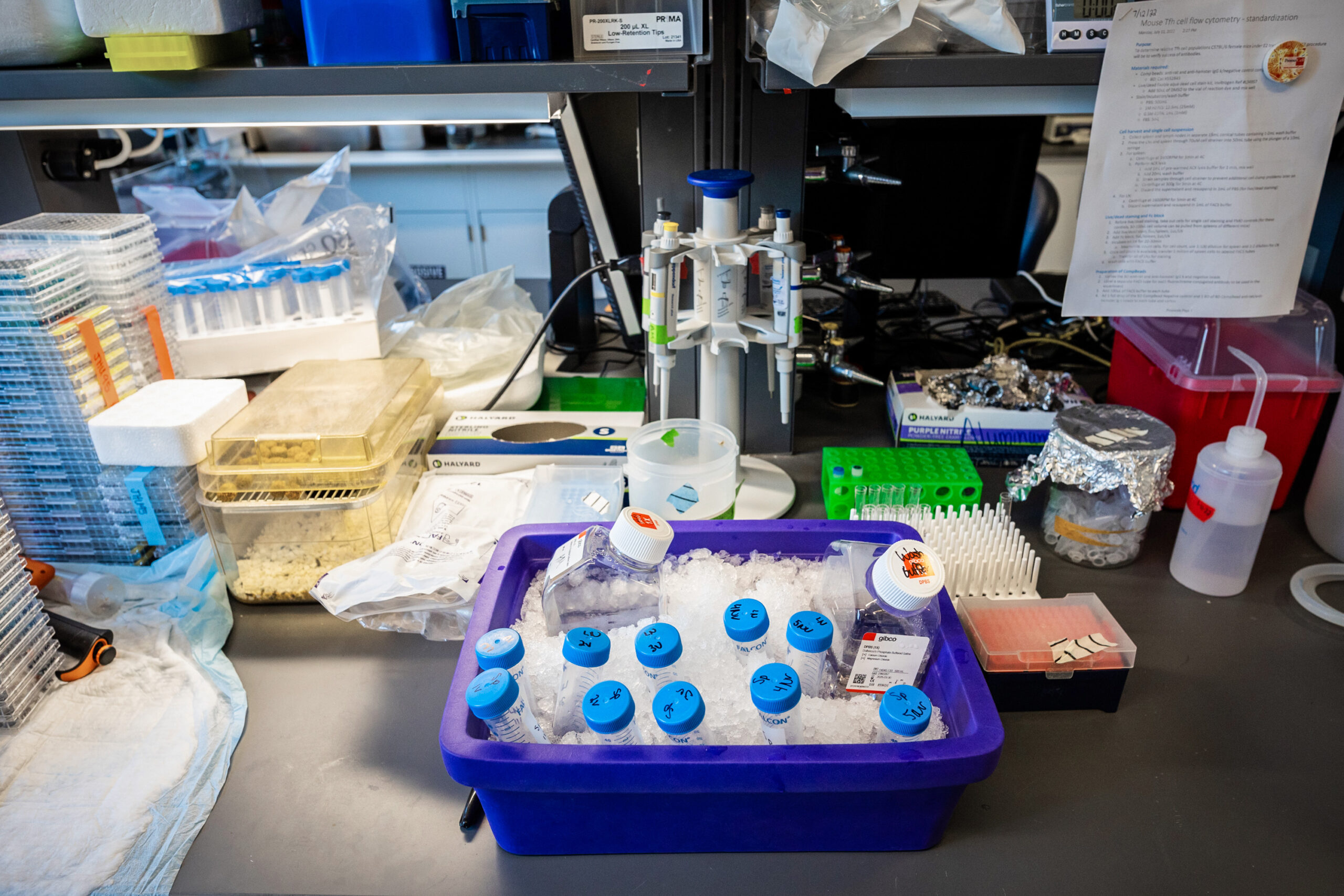
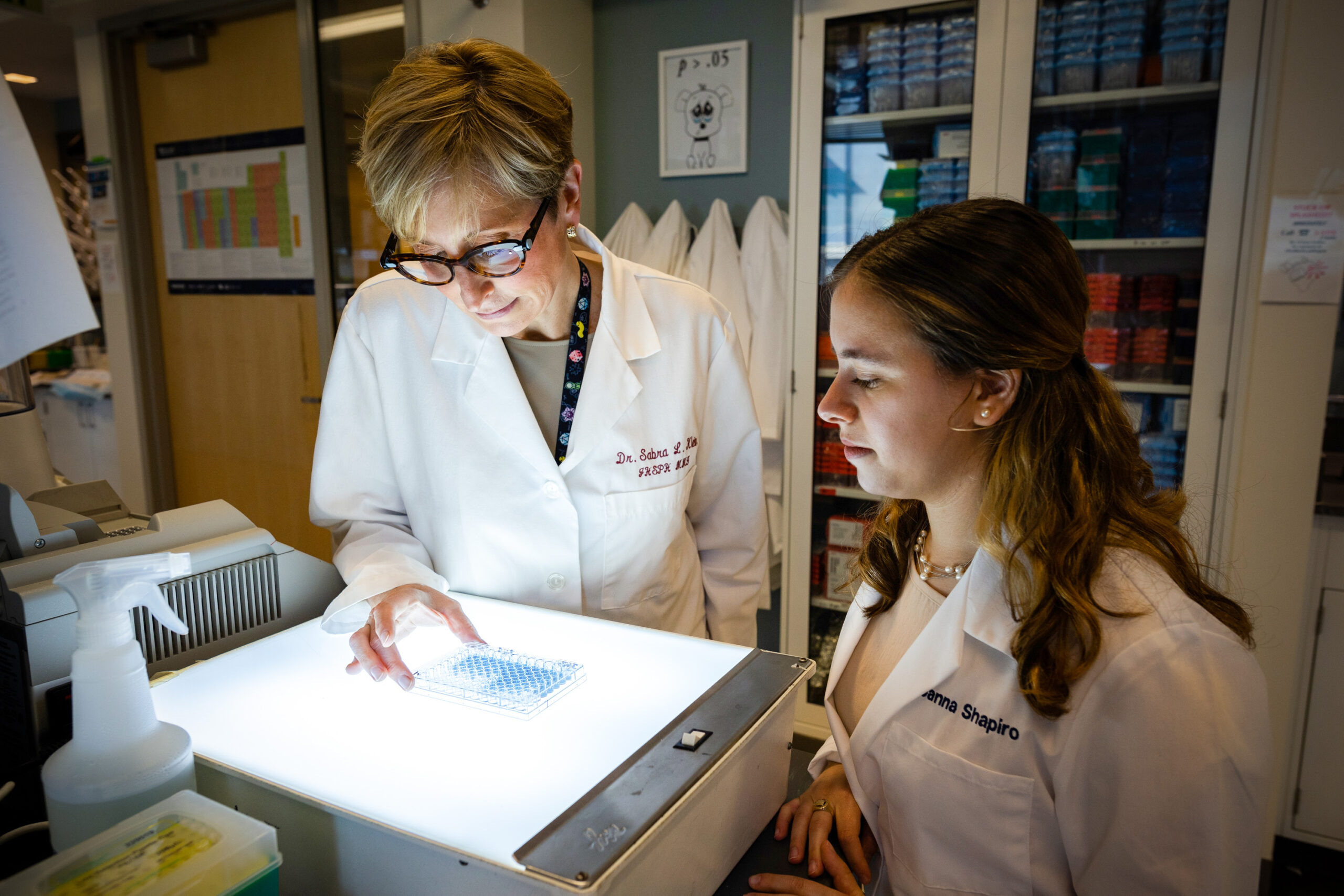
Researchers in Klein’s lab use viruses, immune cells (on ice), and other tools to study sex differences in the immune system.
“That was a major hole in the eligibility of women for therapy,” says Scully. “That’s just an example of how a biomarker—in this case HIV viral load—did not perform in the same way in males and females, and it had a clinically significant impact on treatment recommendation.”
Sex chromosomes also interact with sex hormones such as testosterone, progesterone, and estrogen, and these hormones can themselves directly influence immunity. Just about every immune cell type in your body has receptors that sex hormones can bind to and then regulate gene expression.
Klein has found that estrogen protects female mice against the flu by dampening inflammatory responses and increasing antibody responses to vaccination. These mechanisms may apply to humans as well. “We’ve published studies showing both in younger- and older-aged women that the higher your estrogen level, the better your antibody response to the flu vaccine,” says Klein.
Whether a disease changes after puberty or menopause or during pregnancy can offer clues about the involvement of sex hormones. “Pregnancy is known to be very good for MS patients. It makes them go into remission,” says Voskuhl. She traced this effect to estriol, an estrogen uniquely produced during pregnancy; it has anti-inflammatory and neuroprotective properties. Voskuhl has been testing estriol in clinical trials as a potential treatment against multiple sclerosis, and she says so far results have been promising.
Asthma is another disease where sex hormones seemed likely to play a role, given that its prevalence changes dramatically after puberty. Asthma is more prevalent in boys than girls during childhood, but after puberty it becomes more common and more severe in women than men.
Newcomb has found that in mice, removing androgens—hormones such as testosterone that are dominant in males—increased asthma-associated airway inflammation, whereas removing estrogen signaling decreased asthma. “That told us that estrogens increased and androgens decreased airway inflammation,” she says.
Androgens such as testosterone may be too blunt a tool to serve as a therapy for asthma, but researchers are currently testing the effects of a related hormone, DHEA, that doesn’t have systemic effects. If all goes well, it could be useful not just in preventing asthma, but also in some autoimmune diseases such as lupus and multiple sclerosis.
“There is drastic underrepresentation of gender and sexual minorities in clinical research.”
While there’s plenty left to investigate about the role of sex hormones and sex chromosomes, it’s also becoming increasingly clear that other types of sex differences also play a role—through genes outside the sex chromosomes, for example, and through microbial activity in our digestive systems. The 10 trillion to 100 trillion microbes that reside in our gut and their associated genomes, known as the gut microbiome, also differ between males and females. They are known to influence our immune system and may play a role in greater female susceptibility to autoimmune diseases.
Research into these other mechanisms underlying immunological sex differences is still in its infancy, but the future seems bright. “It’s really a frontier that’s ripe for therapeutics,” says Voskuhl.
For research on sex differences to fulfill its promise for human health, scientists will also have to pay attention to how sex interacts with gender.
The covid-19 pandemic put this need into sharp relief. Early reports out of China in 2020 had suggested that men were more likely to die of covid-19 than women, and initial hypotheses focused on gender differences. “Early on, people were saying it was because of smoking behavior, differences in access to care, all that kind of thing,” says Shapiro.
But as the pandemic spread worldwide, men consistently fared worse in terms of mortality (at least if the effects of race are excluded—a 2021 study found that in some regions Black women died at more than three times the rates of white men and Asian men). “To me that says there’s gotta be something fundamental,” says Klein.
Klein was quick to start looking for mechanisms behind sex differences in covid-19 infection. She found in a hamster model of the disease that males get sicker, have more damage to their lungs, and experience more pneumonia-like symptoms, similar to what was reported in humans.
But interpreting how humans respond to infectious diseases is complicated by sociocultural factors such as race and gender. “Certainly there are behavioral factors: acceptance of masks, vaccine uptake, workplace exposure, all these things that feed into your risk of acquiring disease,” says Scully. Women are more often in positions where they’re exposed to covid infection, whether as nurses, teachers, or caretakers of sick family members.
Researchers are also hoping to better account for the entire gender spectrum, including people who are nonbinary or transgender. “For many reasons, some of which are historical underrepresentation, or maybe not feeling welcome in medical research, there is drastic underrepresentation of gender and sexual minorities in clinical research,” Shapiro says. She and other researchers have been incorporating surveys of gender-related behavior and attitudes into studies to generate gender scores. These assessments could allow scientists to study the influence of gender on health and disease, separate from the effects of biological sex and even self-reported gender identity.
In a rare immunological trial involving transgender people, Scully has started looking at the effects of hormone therapy and gender identity in a cohort of transgender women. “Transgender women in particular are a population at very high risk for HIV acquisition,” she says, “so there’s a real interest in trying to understand what the best treatment options are for them.” Hormone therapy could change an individual’s immune response, but social factors could lead to increased stress and thus also potentially affect immune response. Scully’s goal is to understand these effects and take them into account when studying potential HIV treatments or cures.
There are still groups of people whose immune systems have barely been studied, such as those who are intersex. They can have variations in sex chromosomes, reproductive anatomy, genes, and hormones that do not fit typical notions of male or female bodies.
Not only will a better accounting of sex and gender diversity help increase our knowledge of health and disease for more people, but it might provide fascinating insights into how sex chromosomes, sex hormones, genes, and gender interact to influence the immune system and susceptibility to disease. “We need to look at how men and women and gender minorities are impacted differentially so we can have better health care, better medicine, better vaccines,” says Morgan.
For her part, Klein is hoping to expand the field of sex differences even further. Fresh from putting together the first major symposium on sex differences in the immune response for the American Association of Immunologists in May 2022, she’s organizing a major international gathering of scientists in April 2023, at the first Gordon Research Conference on sex differences in immunology. “I want to learn from people working in cancer, I want to learn from people working in autoimmune diseases, I want to learn from people who are studying immune responses in the brain,” says Klein. “I’m trying to bring us together under this theme of understanding the biology of sex differences, so that we might find some uniform truth or subtle differences across fields.”
The conference will certainly look and feel different from those during Klein’s early days in immunology, when she often felt alone in talking about sex differences. After two decades of work to push these ideas into the mainstream, she says, things have changed: “I think as a field immunology is taking this seriously.”
Sandeep Ravindran is a freelance science journalist based in Bethesda, Maryland.

