Subtotal: 120,88€ (incl. VAT)
A memory prosthesis could restore memory in people with damaged brains
A unique form of brain stimulation appears to boost people’s ability to remember new information—by mimicking the way our brains create memories.
The “memory prosthesis,” which involves inserting an electrode deep into the brain, also seems to work in people with memory disorders—and is even more effective in people who had poor memory to begin with, according to new research. In the future, more advanced versions of the memory prosthesis could help people with memory loss due to brain injuries or as a result of aging or degenerative diseases like Alzheimer’s, say the researchers behind the work.
“It’s a glimpse into the future of what we might be able to do to restore memory,” says Kim Shapiro, a neuroscientist at the University of Birmingham in the UK, who was not involved in the research.
It works by copying what happens in the hippocampus—a seahorse-shaped region deep in the brain that plays a crucial role in memory. The brain structure not only helps us form short-term memories but also appears to direct memories to other regions for long-term storage.
Mimicking memory
For more than 10 years, Theodore Berger and Dong Song at the University of Southern California and their colleagues have been developing a way to mimic this process. Their idea is to use brain electrodes to understand the electrical patterns of activity that occur when memories are encoded, and then use those same electrodes to fire similar patterns of activity.
The team has tested versions of this prosthesis in animals and in some human volunteers with epilepsy who already had electrodes implanted in their brains in order to better understand and treat their condition.
To find out if it might help people with poor memory, Rob Hampson, a neuroscientist at Wake Forest University School of Medicine in North Carolina, and his colleagues tested two versions of the memory prosthesis in 24 people who had implanted electrodes to study their epilepsy, some of whom also had brain injuries.
The first version, which the team calls a memory decoding model (MDM), mimics patterns of electrical activity across the hippocampus that occur naturally when each volunteer successfully forms memories. The MDM model takes an average of these patterns across each individual and then fires off this pattern of electrical stimulation.
The second type, called multi-input, multi-output (or MIMO), more closely mimics how the hippocampus works. In a healthy hippocampus, electrical activity flows from one layer to another before spreading to other brain regions. The MIMO model is based on learning the patterns of electrical inputs and outputs that correspond with memory encoding, and then mimicking them.
Unique brains
To test how well each of the models works, Hampson and his colleagues asked the volunteers to take part in memory tests. In the tests, each person was shown an image on a computer screen. After a delay, the same image was presented again, along with a selection of others. The person had to choose which was the image that had already been shown. Each volunteer completed around 100 to 150 of these short tasks, which are designed to test a person’s short-term memory.
Between 15 and 90 minutes later, each person underwent a second test—this time being shown a set of three images and asked to choose which was most familiar. This test indicates a person’s long-term memory.
The volunteers undertook both rounds of memory tests twice—once to record from the hippocampus, and once to stimulate those recorded patterns associated with successfully stored memories. The recordings were unique, says Hampson: “So far we find that it’s different for each person.”
The team found that its memory prosthesis improved the volunteers’ performances on memory tests—their scores were significantly higher if they had received the correct pattern of stimulation when first presented with the images. This suggests that the memory prosthesis can help encode memories in the brain, the researchers say. “We’re seeing improvements that range from 11% to 54%,” says Hampson.
Personalizing brain stimulation in this way is “a really important thing to be doing,” says Josh Jacobs at Columbia University, who also studies brain recordings from people with epilepsy but was not involved in the current research. So far, doctors and scientists have had some success in treating disorders like Parkinson’s disease by simply targeting the same brain region in all individuals.
“But individuals have really different brain responses,” says Jacobs. Customizing stimulation to individual brains is likely to improve its impact, he says.
The MIMO model, which more closely mirrors how the hippocampus works, had even better results, on average. And the biggest improvements were seen in people who had the worst memory performance at the start of the experiment. The researchers aren’t sure why this is, but it could be because there’s “more room for improvement,” says Hampson.
All the volunteers had their electrodes removed within a couple of weeks, once their doctors had completed investigations into their epilepsy. But Song hopes the improvements to their memories will be lasting. In theory, the stimulation each person received could have strengthened the wiring of neurons in the hippocampus, he says: “We don’t really know, but we hope so.”
Restoring memory
Song, Hampson, and their colleagues, who published their findings in the journal Frontiers in Human Neuroscience in July, hope that their memory prosthesis could one day be widely used to restore memory in people with memory disorders.
“Brain injury patients would be the first [candidates],” says Song. Such injuries tend to affect specific regions of the brain. Injuries to the hippocampus would be easier to target than degenerative diseases like Alzheimer’s, which tend to involve damage across many regions of the brain.
“It seems possible to me that one day we could replace a hippocampus with something else,” says Jacobs. But he points out that it will be difficult to fully replicate a healthy hippocampus—the structure contains tens of millions of neurons. “It is a little hard to imagine how a handful of electrodes could be replacing the millions of neurons in the hippocampus,” he says.
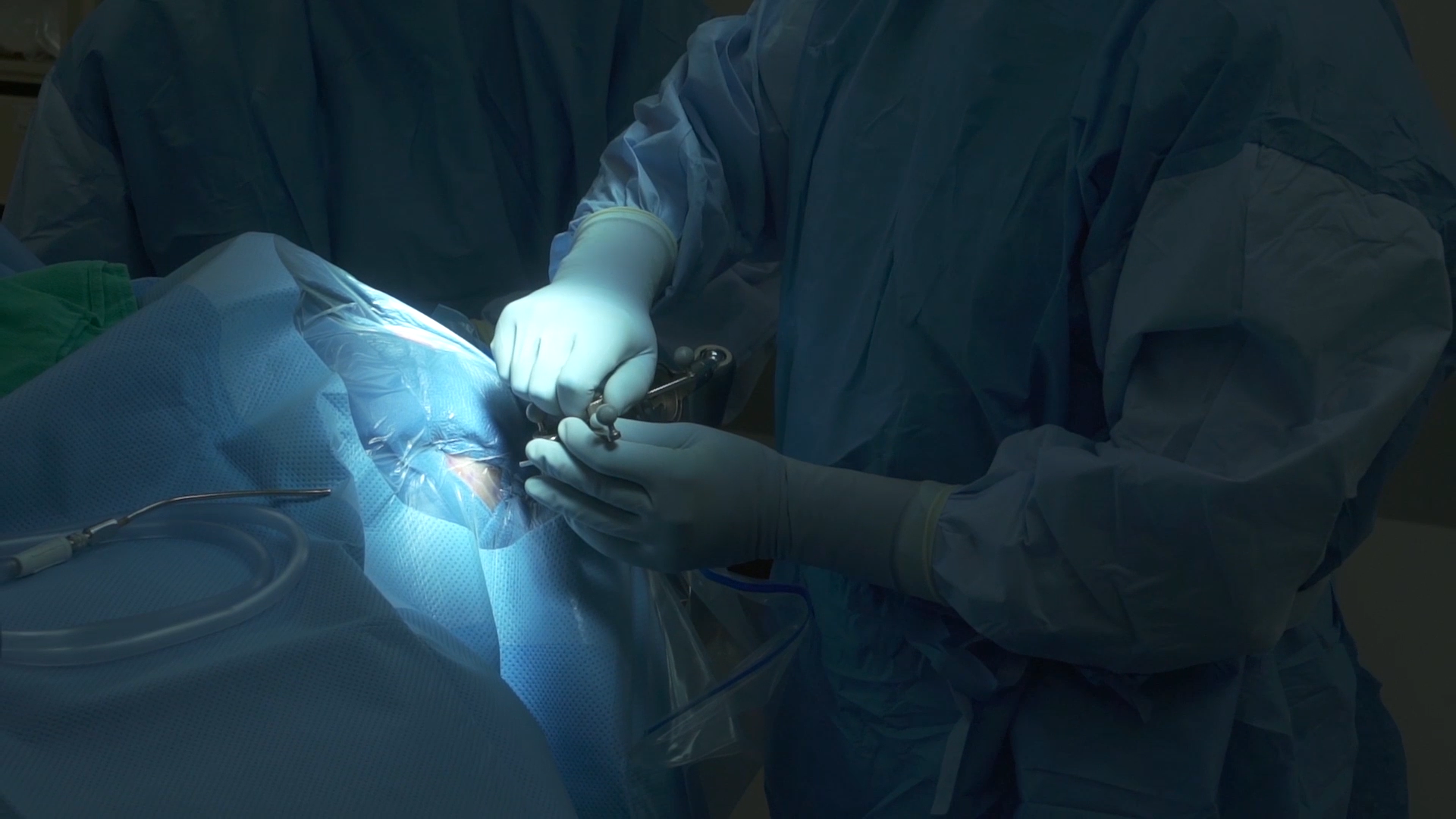
WAKE FOREST MEDICAL CENTER
The electrodes used in the study are around a millimeter wide, and all the volunteers had them implanted deep enough into the brain to reach the hippocampus—around 10 centimeters deep. They are fairly crude by modern research standards and are only able to record from around 40 to 100 neurons, says Song. Any memory prosthesis designed to treat memory disorders will require brain electrodes with hundreds of contact points, allowing them to record from, and stimulate, hundreds or thousands of neurons, he says.
Hampson, Song, and their colleagues haven’t yet worked out how the memory prosthesis might work in practice. It might not make sense to have the device running all the time, for example—there are plenty of life experiences, such as taking out the garbage, that people with memory disorders don’t need to remember. “Why waste the [brain] space?” Jacobs says.
Song thinks the prosthesis might be used alongside some sort of device that can tell whether the device needs to be running or not—perhaps by detecting when the brain needs to be in a ready-to-learn state.
And Song doesn’t yet know if a memory prosthesis should run overnight, either. It is thought that when we sleep, the hippocampus replays some of the memories encoded during the day, in order to consolidate them in other brain regions. Song and his colleagues don’t know if a memory prosthesis that replicates this replay would improve memory, or whether it’s a good idea to stimulate the hippocampus at all while a person is sleeping.
Either way, the prosthesis is still some way from clinical use, says Shapiro. “I think in principle it could work,” he says. “[But] we have a long way to go before we understand enough about memory to be able to use this sort of approach to replace hippocampal function.”


